
When we’re sick, we want to do all we can to feel better. Infections are due to germs, including viruses, bacteria, and fungi. Often, people equate being sick with needing an antibiotic. This is usually NOT true! In fact, when not needed, antibiotics do more harm than good! Antibiotics can help if, and only if, the infection is due to bacteria. For infection due to viruses, which are far more common, antibiotics are of no benefit. Antibiotics cause harm in three ways: (1) they kill the “good” protective bacteria in our gut, which predisposes to something called C diff (see below); (2) antibiotic use leads to the emergence of antibiotic resistance, which renders them ineffective for future use; and (3) antibiotics can cause unwanted side effects such as rash, nausea, and diarrhea. Antibiotics account for almost 14% of all adult emergency room visits for adverse drug events!
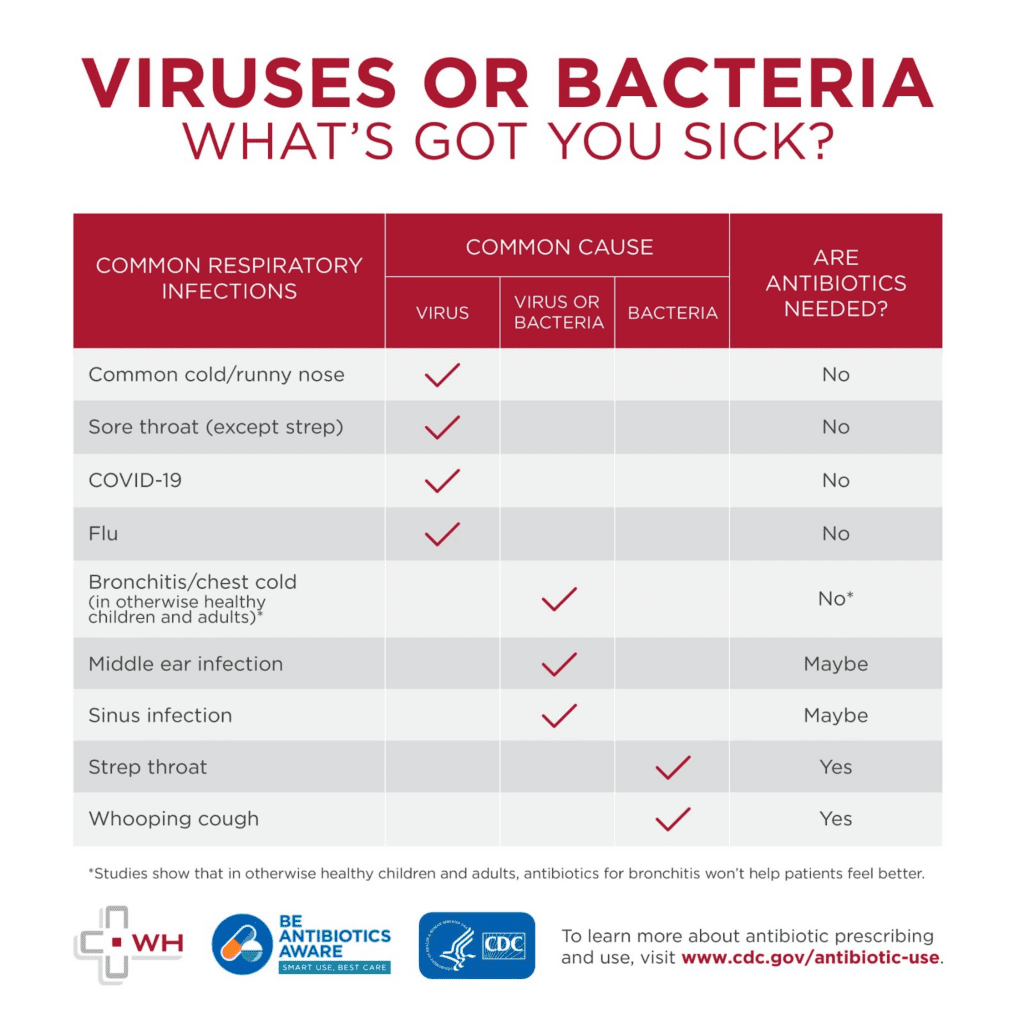
How do you know if you need antibiotics?
All of the following infections are due to viruses, and antibiotics should not be given to treat them:
- Common colds, runny noses (even with thick, discolored mucus)
- Bronchitis, in those without COPD
- Covid-19 (although antiviral medicines may be helpful)
- Flu (although antiviral medications may be helpful)
- Sore throat not proven to be due to Strep
- Most cases of sinusitis
- Most ear infections
Can bacterial infection follow an initial viral infection?
Yes, but only in a small minority of cases. Respiratory viruses usually run their course over a matter of days. An exception to this is bronchitis, where cough may persist for weeks following viral infection, without secondary bacterial involvement or need for an antibiotic. Your provider may prescribe cough medicine, or sometimes an inhaler, to help with these symptoms. In other cases, time – i.e., the duration of symptoms, is a helpful determining factor. For example, if you have sinus congestion (sinusitis) that continues for 10 days or more, an antibiotic may be helpful. Other potential signs of bacterial infection include high fever, or an elevated white blood cell count.
You can help prevent viruses from spreading with a few precautions:
- Avoid close contact with people who have colds or other upper respiratory infections
- Cover coughs
- Don’t touch your eyes, nose, and mouth with unwashed hands
- Remain home when you’re sick
- Stay up to date on vaccines, including those for influenza
- Wash hands with soap and water for at least 20 seconds, and/or use an alcohol-based hand sanitizer.
What is antibiotic resistance?
Antibiotic resistance emerges when bacteria that live within our body are exposed to antibiotics. When we take an antibiotic, bacteria we harbor that are susceptible to the antibiotic are killed. However, some bacteria harbor genes, known as resistance genes, that allow them to survive. The resistant bacteria are then able to grow, reproduce, and then dominate the bacterial population. Resistance genes encode a wide variety of mechanisms rendering antibiotics ineffective. For example, some bacterial resistance genes code for proteins that actually chemically destroy the antibiotic. It’s important to understand that humans did not actually “invent” antibiotics. Bacteria have been making and using substances akin to antibiotics against each other for billions of years in their struggle to compete with other bacteria and survive in nature. It’s currently thought that resistance genes against every antibiotic produced by humans, now or in the future already exist in nature. Bacteria readily share these genes amongst each other, such that many bacterial species already carry them. When bacteria don’t need these genes to survive, they “shut them off”. But when bacteria are exposed to antibiotics we take, the resistance genes are “turned back on” as part of the bacteria’s struggle to survive. The only way to prevent emerging antibiotic resistance is to use antibiotics sparingly, and only when necessary. Every year, 2.8 million Americans contract antibiotic-resistant infections, and more than 35,000 cases are fatal.
Tips for taking antibiotics
- Antibiotics are effective for people who need them — those with bacterial infection — and may be life-saving. Do not ask for, or expect antibiotics when sick with viral infections that account for most respiratory illnesses.
- Take antibiotics exactly as prescribed, even if you start to feel better.
- Never save antibiotics for later infections, and don’t share them with anyone. Your provider should prescribe the least amount of antibiotics, and only when clearly indicated. This can help improve health while reducing antibiotic resistance risk.
Side effects to watch for
Side effects can be minor to severe. Among the most common are:
- Diarrhea
- Dizziness
- Nausea
- Rash
- Yeast infections
- Serious side effects warrant medical attention, such as:
- Severe diarrhea. It could signal a C. diff infection (see below), which can cause severe damage to the colon and lead to death.
- Life-threatening allergic reactions. These include:
- Anaphylaxis (feeling that your throat is closing or choking, or your voice is changing)
- Hives
- Shortness of breath
- Wheezing
Careful use of antibiotics can help assure their effectiveness in the future. Speak with your provider if you have questions about antibiotic use. Disclose any other medications you take to check for possible interactions with antibiotics. Report possible side effects to your physician right away.
What is a C. diff infection?
C. diff is a bacteria that produces toxins which may lead to severe and even life-threatening diarrhea. Antibiotics are the leading predisposing cause of C. diff. When antibiotics are taken, many the normal “good” bacteria in our gut are killed off. It may take up to two years for these “good” bacteria to re-populate our gut — even after a single course of antibiotics! In this setting when the “good” bacteria are depleted, C. diff may take advantage of this situation by over-growing and producing toxins leading to diarrhea. Mild diarrhea is common after taking antibiotics. But if you develop multiple episodes (3-20) of watery diarrhea per day in the wake of taking an antibiotic, you should promptly contact your provider regarding submitting a stool sample to test for C. diff infection.
Antibiotics and children
Kids can recover from many illnesses without antibiotics. Check with your provider about your options.
Antibiotics should be used to treat the infection with minimal side effects. The Food and Drug Administration (FDA) advises against prescribing fluoroquinolones. These are a type of antibiotic linked to C. diff infections, which should not be considered a final option.
Often, other measures can help reduce children’s symptoms, such as:
- Fever reducers
- Liquids
- Pain relievers
- Rest
- Saline nasal spray or drops
- Warm compresses
Antibiotics and nursing home residents
More than 3 million Americans get care in or live in nursing homes each year. Antibiotics help treat conditions such as pneumonia and sepsis, and severe responses to infections by the body.
Antibiotics at the dentist
Antibiotics are given prior to dental work to prevent infection caused by mouth bacteria that gain entry into the bloodstream, particularly in patients with artificial heart valves. For those with artificial joints (hips, knees, shoulders), however, antibiotics for dental work is NOT advised.
Tips for good dental health
The most effective way to avoid antibiotics is to not need them. Also:
- Brush your teeth twice daily with fluoride toothpaste
- Don’t use tobacco
- Drink fluoridated water
- Floss daily to remove plaque
- Visit your dentist at least once a year, even if you have no natural teeth or have dentures
Do you have more questions about antibiotic use?
You can always talk to your primary care physician at Wilmington Health. At the time your condition requires treatment or at any point of your health journey, count on TRUE Care from Wilmington Health.
